Medicines have been essential throughout human history, helping us fight diseases and greatly improving the quality of life for people worldwide.
In this blog, we will explore in depth what medicines are and how they have evolved throughout history. We will look at the fascinating process of their creation, from research and development to production and distribution. In addition, we will discuss the impact they have on our society, both from a public health and an economic perspective. Our aim is to provide an understandable and comprehensive overview of drugs, highlighting their importance and the scientific rigour behind their development.
What are Medicines?
Medicines are products we use to treat, prevent or diagnose diseases in people and animals. They can come in different forms, such as pills, capsules, liquids, injections and creams. In other words, they are tools to help us feel better when we are sick or to keep us healthy.
From a more scientific perspective, medicines are substances or combinations of substances designed to interact with the body at the molecular and cellular level. They can be synthetic chemical compounds, produced in laboratories, or biological compounds, derived from living organisms. Drugs work in a variety of ways, such as inhibiting enzymes, blocking receptors, or modifying gene expression, to correct physiological imbalances or eliminate pathogens.

Types of medicines
- Anti-infective agents: These include medicines that treat bacterial, viral and fungal infections.
- Central nervous system agents: These include drugs that affect the brain and spinal cord to treat pain, psychological disorders and improve attention.
- Cardiovascular agents: Used to treat conditions of the heart and circulatory system, such as hypertension and heart rhythm problems.
- Endocrine agents: These include hormone-regulating drugs to treat diabetes, thyroid disorders and reduce inflammation.
- Gastrointestinal agents: These include medicines that relieve stomach problems and improve digestion.
- Antineoplastic agents: Used to treat cancer by inhibiting the growth of cancer cells or by blocking hormones that promote cancer.
- Immunological agents: Medicines that modify the immune response, such as immunosuppressants, or prevent disease through vaccines.
- Respiratory agents: Treat respiratory conditions by facilitating breathing or combating allergies.
How medicines are made
Developing drugs is a long and expensive process, taking 10-15 years and costing millions of dollars.

1. Research and Development (R&D)
Drug discovery
The first step in the creation of a new medicine is drug discovery. This process begins with the identification of a disease or condition in need of treatment. Scientists look for biological 'targets', which are molecules in the body involved in the disease. These targets may be proteins, genes or cellular structures.
Discovery methods
- High-Throughput Screening (HTS): A technique that allows researchers to rapidly test thousands of chemical compounds to identify those that interact with the biological target.
- Structure-Based Drug Design: Uses computational models to design molecules that specifically fit the biological target.
- Systems biology: A comprehensive approach that uses genomics, proteomics and metabolomics data to understand how different parts of a biological system interact and how they may be influenced by drugs.
Lead optimisation
Once potential compounds are identified, the lead optimisation phase begins. Lead compounds are those that show the most promise in initial trials. These compounds are chemically modified to improve their efficacy, reduce toxicity and optimise their pharmacokinetic properties (how they are absorbed, distributed, metabolised and eliminated in the body).

2. Pre-clinical studies
In Vitro Tests
Before testing compounds in animals or humans, in vitro tests are performed. These tests are carried out on cells grown in the laboratory and aim to assess the toxicity and efficacy of the compounds.
In Vivo Rehearsals
If in vitro tests are promising, compounds are tested in animals to study their effect in a living organism. These in vivo tests help to identify any adverse effects and to determine the appropriate dose.
3. Clinical trials
Phase I: Initial Security Assessment
The first phase of clinical trials involves a small group of healthy volunteers (usually between 20 and 100 people). The main objective is to assess the safety of the drug and to determine the maximum tolerated dose. Researchers also monitor side effects and how the body metabolizes the drug.
Phase II: Effectiveness and Safety
In Phase II, the drug is tested in a larger group of several hundred people, who have the target disease or condition. This phase is often divided into Phase IIa (initial assessment of efficacy and dose) and Phase IIb (confirmation of efficacy and safety). The data collected in this phase help to refine the dose and identify any additional side effects.
Phase III: Large Scale Trials
Phase III involves thousands of patients and is conducted at multiple clinical sites. These trials are crucial to confirm the efficacy of the drug and monitor long-term side effects. In addition, phase III trials compare the new drug with existing standard treatments, if available.
4. Approval and regulation
Submission of Application
If Phase III clinical trials are successful, the pharmaceutical company submits an application for approval to the regulatory authorities. In the US, this application is called a New Drug Application (NDA) and is submitted to the FDA. In Europe, a similar application is submitted to the EMA.
Regulatory Review
Regulatory authorities review all pre-clinical and clinical trial data, as well as information on the manufacture and labelling of the medicine. This process can take several months or even years. If regulators are satisfied with the safety and efficacy of the drug, they will grant marketing approval.
5. Production and Manufacturing
Chemical or Biological Synthesis
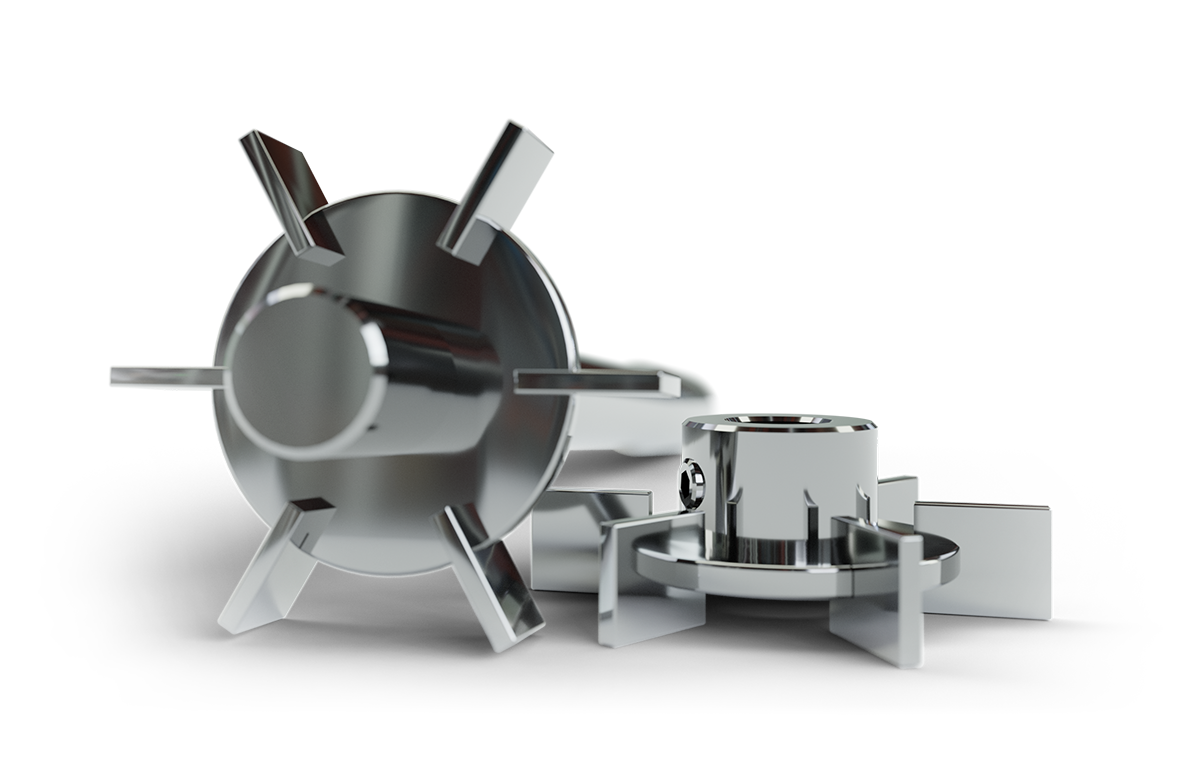
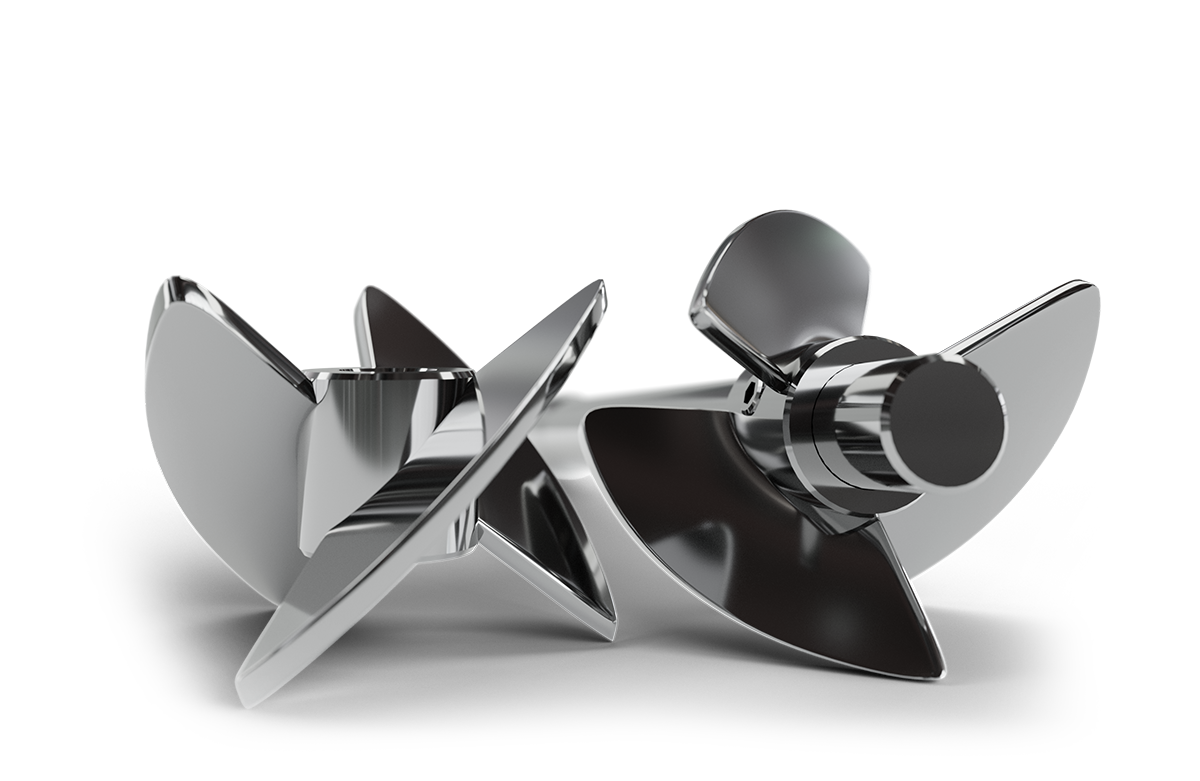
The production of drugs begins with the synthesis of the active ingredient. For chemical medicines, this involves controlled chemical reactions under specific conditions. Biological medicines, such as monoclonal antibodies, are produced using live cells grown in bioreactors ⇀, where conditions such as nutrients and temperature are carefully controlled. Subsequently, tangential flow filtration systems ⇀ is used for concentration and purification of these products, ensuring their quality and effectiveness.
Formulation
Once the active ingredient has been produced, it is mixed with excipients (inactive substances) to create the final dosage form, such as capsules, liquids or injections. The formulation must ensure that the medicine is properly released into the body and is stable throughout its shelf life.
Quality Control
Each batch of medicine produced undergoes rigorous quality controls to ensure that it meets established specifications. These controls include tests for purity, potency, stability and freedom from contaminants.
Packaging and Distribution
The final medicine is packaged in sterile conditions and labelled with information on its use, dosage and warnings. It is then distributed to hospitals, pharmacies and other outlets.
Post-marketing
Once a drugs is on the market, safety surveillance continues through pharmacovigilance. Manufacturers and regulatory authorities monitor adverse event reports and conduct post-marketing studies to identify any long-term safety issues.
Over time, adjustments may be made to the formulation or manufacture of the medicine to improve its efficacy, safety or stability. In addition, new indications for the drug may be developed, extending its use to other diseases or conditions.

Impact of medicines on society
Medicines help people stay healthy by treating infections, managing long-term illnesses, and improving longevity and quality of life. Vaccines have eradicated diseases such as smallpox and significantly reduced the incidence of many others.
The pharmaceutical industry is an important economic driver, generating employment and contributing to research and development. However, it also faces challenges such as high development costs and concerns about access and affordability of medicines.
Continuous innovation marks the future of medicines. Personalised medicine, cell and gene based treatments, and new technologies such as artificial intelligence are revolutionising the way researchers discover and develop drugs. These innovations promise more effective and personalised treatments, tailored to the specific needs of patients.
Conclusion
Medicines have come a long way from ancient times to the modern era, and they continue to evolve. Their development and production are complex processes that require years of research and rigorous testing. However, the positive impact they have on the health and well-being of mankind is undeniable. In the future, biotechnology and innovation will be important for making medicine better and improving quality of life.
Frequently Asked Questions (FAQ)
Medicines are products that we use to treat, prevent or diagnose diseases in people and animals. They can come in different forms, such as pills, capsules, liquids, injections and creams.
Medicines interact with the body at the molecular and cellular level to correct physiological imbalances or eliminate pathogens. They may inhibit enzymes, block receptors or modify gene expression.
After clinical trials, the pharmaceutical company submits an application for approval to regulatory authorities, such as the FDA in the US or the EMA in Europe. These authorities review the data and, if satisfied with the safety and efficacy of the drug, grant marketing approval.
The main advantage of a bioreactor is its versatility and ability to handle a variety of biological processes with strictly controlled culture conditions.
Artificial intelligence and other emerging technologies are revolutionising drug development by accelerating the drug discovery process, optimising clinical trials and personalising treatments..